Heart Racing After Eating: Should You Worry or Just Skip Dessert?
You sit down, enjoy a meal, life is good… and then your heart suddenly feels like it’s auditioning for a drum solo. Fast heartbeat. A weird thump in your chest. Maybe a little shaky or anxious on top. And now you’re wondering: “Is this normal, or do I need to head to the ER?”
Let’s walk through what might be going on when your heart races after eating, what’s usually harmless, what’s not, and how to calm things down without spiraling on WebMD.
What Does “Heart Racing After Eating” Actually Mean?
When people say their “heart is racing after eating,” they usually mean one or more of these:
- Fast heart rate (tachycardia): resting heart rate jumps above about 100 beats per minute shortly after a meal.
- Pounding or fluttering sensations (palpitations): you feel your heartbeat in your chest, neck, or even ears.
- Skipped beats or extra beats: the heart feels like it “drops” or “kicks,” often from benign extra beats.
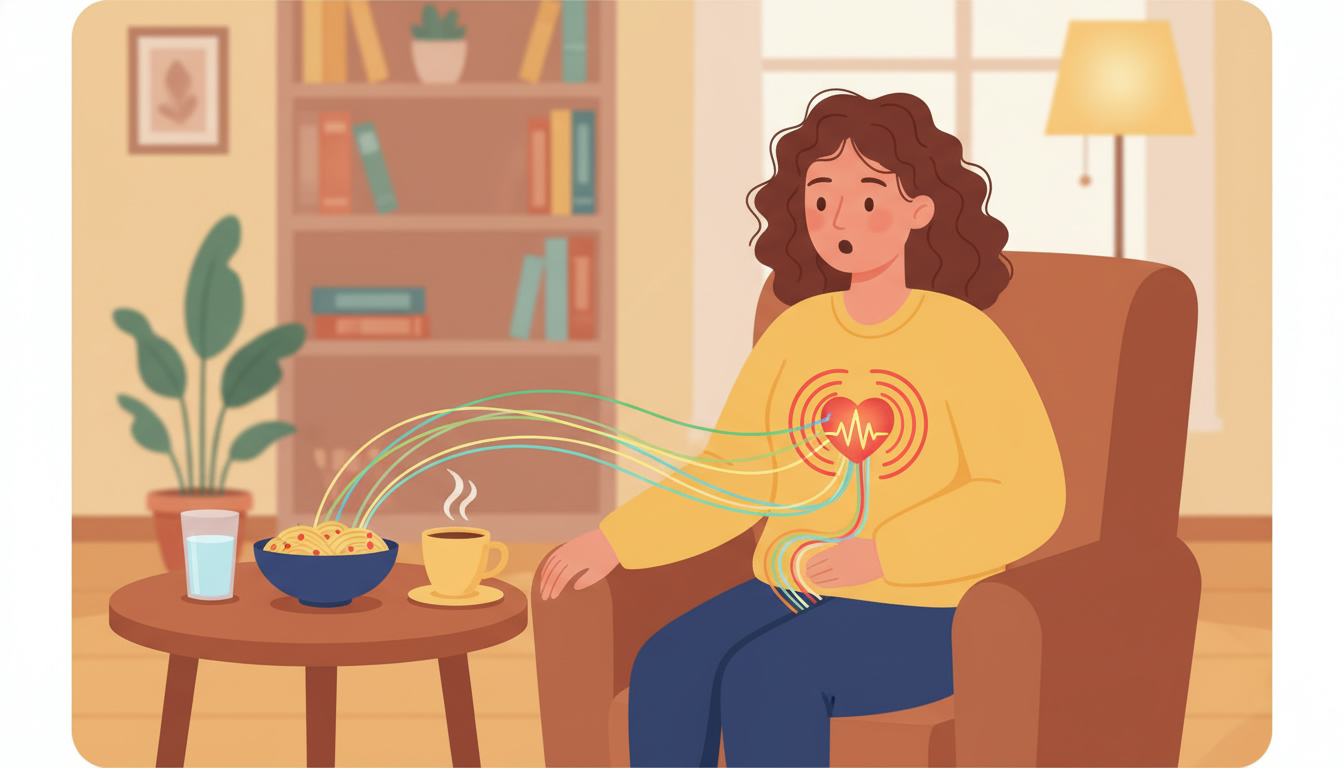
A small increase in heart rate after eating is normal. Your body is sending more blood to your digestive system and activating what’s called the “rest and digest” response.
The problem is when it feels sudden or intense, it comes with other symptoms such as chest pain, shortness of breath, or faintness, or it happens frequently or seems to be getting worse over time.
Takeaway: A little bump in heart rate after a meal is common. Big, scary jumps or scary symptoms deserve attention.
Common (Often Harmless) Reasons Your Heart Races After Eating
There are several everyday triggers that can make your heart pound post-meal. These are very common and usually not dangerous on their own, but they are still worth paying attention to.
1. Large, Heavy, or High-Carb Meals
When you eat a big meal, especially one heavy in refined carbs, sugar, or fat, your body has to work harder to digest it. Blood flow shifts to your digestive tract, and your heart may beat faster to keep up.
Think:
- Big pasta dinner
- Huge fast-food combo
- Holiday buffet “I regret everything” plate
If your blood sugar spikes quickly from lots of simple carbs or sugar, your body releases insulin to bring it down. Rapid blood sugar swings can trigger a racing heart in some people, along with shakiness or lightheadedness.
What this feels like:
- Fifteen to forty-five minutes after eating, your heart feels faster or more noticeable.
- You might feel sleepy, a bit sweaty, or “off.”
Takeaway: Big, carb-heavy meals are a classic “heart racing after eating” trigger. Smaller, balanced meals usually stress your system less.
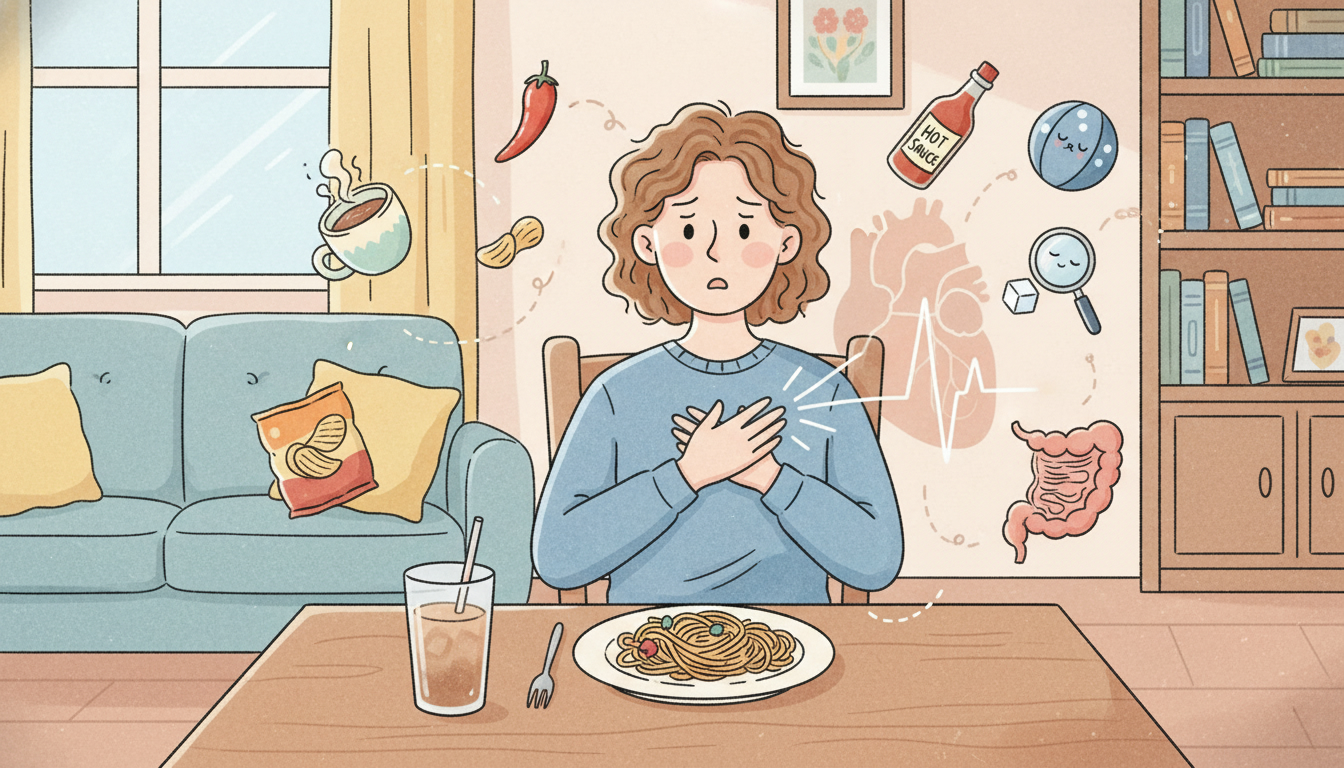
2. Caffeine and Stimulants (Not Just Coffee)
Caffeine stimulates your nervous system and can increase heart rate. If your meal includes coffee or espresso, strong tea or energy drinks, pre-workout supplements, chocolate, or caffeine-containing sodas, it can all add up.
Some people are especially sensitive, and combining caffeine with sugar, such as in sweetened iced coffee or energy drinks, is a double effect.
Takeaway: If your meals plus caffeine lead to a racing heart, experiment with cutting back or spacing caffeine away from meals.
3. Alcohol With Meals
Alcohol can dilate blood vessels, lowering blood pressure, trigger an increase in heart rate to compensate, and act as a direct irritant to the heart’s electrical system in some people.
There is even a term sometimes used informally, “holiday heart,” for heart rhythm issues or palpitations after heavy drinking, even in people without known heart disease.
Takeaway: If your heart pounds after dinner with wine or cocktails, alcohol might be a key player.
4. Dehydration and Electrolyte Imbalances
If you are even mildly dehydrated, your heart may beat faster to maintain blood flow. Combine that with a big meal or salty food, and your cardiovascular system is juggling a lot at once.
Low levels of certain electrolytes like potassium or magnesium can also contribute to palpitations or abnormal beats.
Clues this might be you:
- Dark urine, dry mouth, or headache
- You have had vomiting, diarrhea, or intense sweating recently
- You take medications like diuretics (water pills)
Takeaway: Drink enough water through the day, not just during meals, and talk to a healthcare professional if you suspect electrolyte issues.
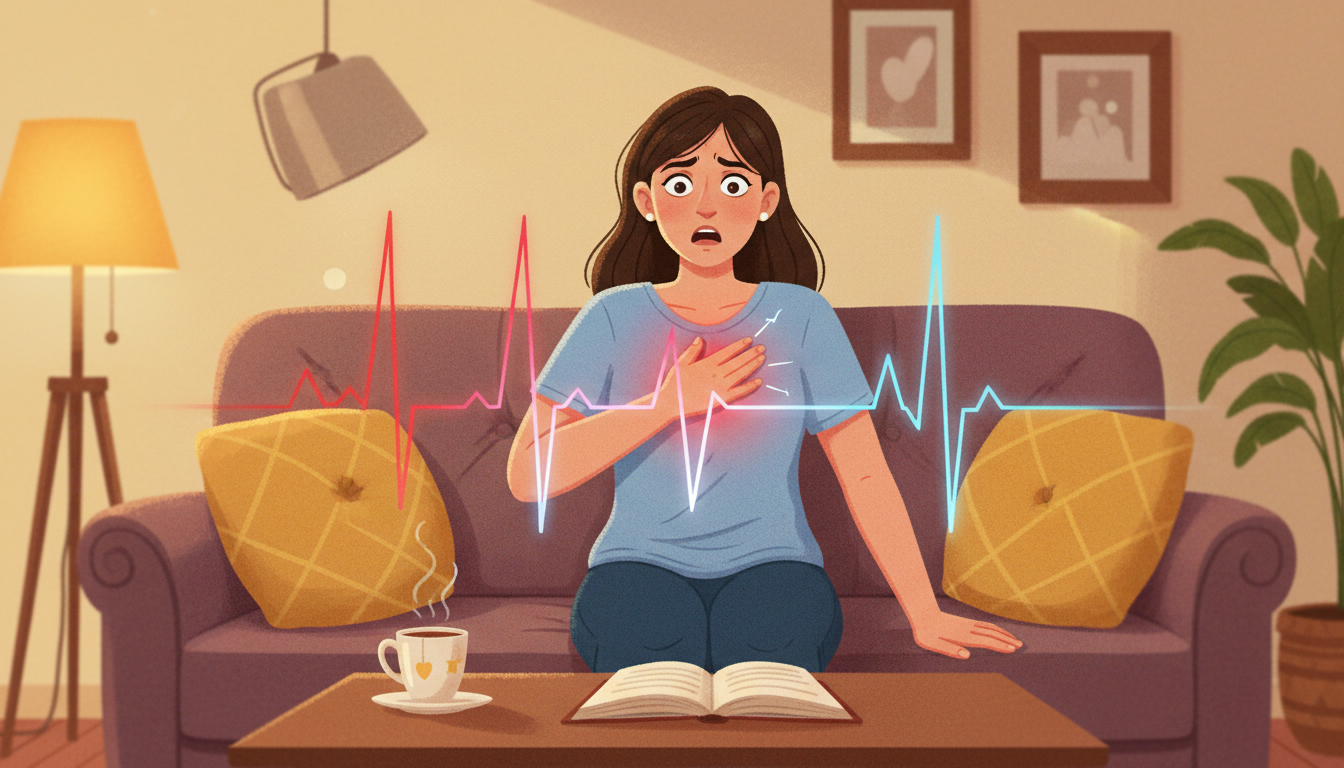
5. Anxiety, Stress, and the “Oh No, What Is This?” Spiral
If you have ever felt your heart race, then immediately felt more anxious, which made your heart race even more, you know the feedback loop.
Anxiety can increase adrenaline, raise heart rate, and make you hyper-aware of normal body sensations. Sometimes, the original trigger might be mild, such as a small bump in heart rate from a meal, but anxiety magnifies it into a full-blown symptom episode.
Takeaway: Your mind and body are a team. Managing stress and anxiety can reduce how intense or scary post-meal heart sensations feel.
Medical Reasons Your Heart May Race After Eating
Now let’s talk about when a racing heart after eating might be part of a bigger medical picture. None of this is a diagnosis, but it is helpful to know what doctors consider.
1. Reactive Hypoglycemia (Blood Sugar Drops After Meals)
In some people, blood sugar may drop too low a few hours after eating, particularly after a carb-heavy meal. This is called reactive hypoglycemia.
Symptoms can include:
- Racing or pounding heart
- Shakiness
- Sweating
- Hunger or nausea
- Feeling suddenly weak or anxious
If you notice you feel worse one to three hours after eating, especially after sugary or high-carb meals, this is worth mentioning to your doctor.
Takeaway: It is not just high blood sugar that causes issues. Big swings up and down can make your heart race too.
2. Postprandial Hypotension (Blood Pressure Drop After Eating)
Postprandial simply means “after a meal.” In postprandial hypotension, your blood pressure drops after eating because blood rushes to your digestive system, and your body does not compensate well.
Your heart may then beat faster to keep blood flowing.
Common symptoms include dizziness or lightheadedness after meals, weakness or feeling like you might pass out, blurry vision, and a racing heart.
This happens more often in older adults or people with certain conditions like Parkinson’s disease, diabetes, or nervous system disorders, but it can occur in others as well.
Takeaway: If you feel dizzy and your heart is racing after eating, especially when standing up, talk to a doctor about your blood pressure.
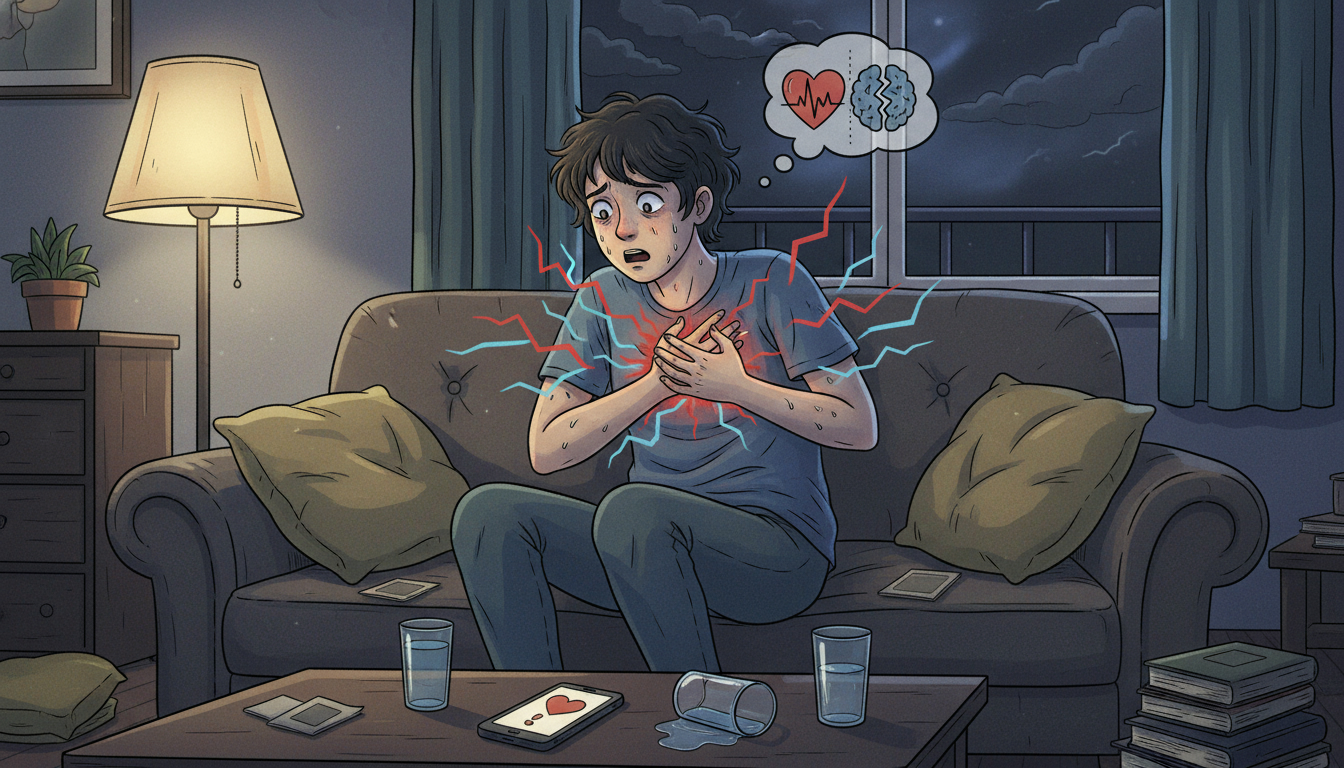
3. Heart Rhythm Issues (Arrhythmias)
Some arrhythmias, or irregular heart rhythms, can flare up around mealtimes.
Examples include:
- Supraventricular tachycardia (SVT): very rapid heart rate that can start and stop suddenly.
- Atrial fibrillation (AFib): irregular, often fast heartbeat that may be noticed more after certain triggers like alcohol, big meals, or caffeine.
Signs this might be more than just a busy digestive system include a sudden racing heart that feels very fast and does not settle within a few minutes, feeling faint, weak, or very short of breath, or an irregular, chaotic-feeling heartbeat.
Takeaway: Intense, sudden, or irregular heart racing, especially with other symptoms, should be checked out urgently.
4. Thyroid Problems
An overactive thyroid (hyperthyroidism) can cause a rapid or pounding heart, anxiety or irritability, weight loss despite normal or increased eating, and heat intolerance and sweating.
When your baseline heart rate is already high from thyroid overactivity, meals and digestion may push it even higher.
Takeaway: If your heart races frequently, not just after eating, ask about thyroid testing.
5. Food Sensitivities, Allergies, and Histamine
Some people notice heart racing or palpitations after certain foods, especially foods they are allergic or sensitive to, or high-histamine foods such as aged cheeses, wine, smoked meats, or some fermented foods.
More severe allergic reactions can cause hives, swelling, wheezing, trouble breathing, tightness in the throat, and a drop in blood pressure. This is a medical emergency and needs immediate attention.
Takeaway: If specific foods reliably trigger symptoms, keep a log and discuss this with a professional, especially if other allergy symptoms show up.
Is It Dangerous If Your Heart Races After Eating?
It can be, but often it is not.
More likely to be benign if:
- It is mild and short-lived, lasting a few minutes.
- It improves when you stand up, walk, or take a few slow breaths.
- You have had a normal heart evaluation in the past and no other symptoms.
More concerning if:
- You have chest pain, tightness, or pressure.
- You are short of breath at rest.
- You feel faint, confused, or actually pass out.
- You have known heart disease, high blood pressure, or diabetes.
- The rhythm feels very irregular or extremely fast.
Bottom line: When in doubt, especially with severe or new symptoms, it is much better to overreact and get checked than to underreact.
Simple Things You Can Try at Home (Non-Emergency Situations Only)
These are general lifestyle tips, not medical treatment, but they help many people calm post-meal heart racing.
1. Shrink Your Meal Size
Instead of two or three huge meals, try four or five smaller meals or snacks. Balance protein, healthy fat, and fiber at each meal to blunt blood sugar spikes.
Example: Swap a giant plate of white pasta and garlic bread for a smaller portion of pasta with grilled chicken or tofu, vegetables, and a side salad.
2. Go Easy on Sugar and Refined Carbs
High-sugar foods and drinks can cause rapid swings in blood sugar and insulin.
Try to cut back on soda, energy drinks, and large desserts, choose whole grains and fiber-rich carbs, and pair carbs with protein and fat, such as an apple with peanut butter instead of just apple juice.
3. Watch the Caffeine and Alcohol Combo
If you suspect caffeine or alcohol is a trigger, move coffee to earlier in the day or reduce the dose, skip energy drinks especially with meals, and limit alcohol and see if episodes improve.
You do not have to quit everything forever, but a two to four week experiment can tell you a lot.
4. Hydrate and Support Electrolytes
Aim to drink water regularly through the day, not only when you are already thirsty. If you sweat a lot, are very active, or take certain medications, ask your doctor if an electrolyte drink or supplement makes sense for you.
5. Gentle Movement After Eating
Instead of collapsing on the couch, take a slow 10 to 15 minute walk or do light stretching. This can help digestion and keep your cardiovascular system balanced.
6. Calm Your Nervous System
If anxiety is in the mix, try slow, deep breathing such as inhaling for four seconds, holding for two, and exhaling for six to eight, box breathing with a four-four-four-four pattern, or grounding by looking around and naming several things you can see, feel, and hear.
Takeaway: Small, consistent tweaks to what and how you eat can significantly reduce after-meal heart symptoms.
When You Should Call a Doctor (Or 911)
Call Emergency Services Right Away if:
- Your heart is racing and you also have chest pain or pressure.
- You have trouble breathing.
- You have pain radiating to jaw, arm, or back.
- You have sudden confusion, trouble speaking, or weakness on one side.
- You faint or nearly faint.
Do not drive yourself if you feel like you might pass out.
Make an Appointment With Your Healthcare Provider Soon if:
- Your heart often races after eating, even with small meals.
- You feel dizzy, weak, or “off” after meals.
- There is a clear pattern with certain foods, but no obvious allergy.
- You have other ongoing symptoms such as weight loss, fatigue, anxiety, tremors, or frequent sweating.
- You have a history of heart issues, high blood pressure, or diabetes.
They might ask detailed questions about your meals and symptoms, check your vital signs, heart, and possibly blood pressure lying versus standing, and order tests like an EKG, Holter monitor, blood work including thyroid and glucose, or an echocardiogram.
Takeaway: You are not bothering anyone by asking about this. Recurrent heart symptoms are exactly the kind of thing worth a professional opinion.
How to Track Your Symptoms (So Your Doctor Can Actually Help)
If your heart races after eating but you are not sure why, a simple log can be incredibly useful.
For one to two weeks, note the time and content of each meal or snack, caffeine and alcohol intake including amount and time, the approximate time symptoms start after eating, what you feel such as fast heart, skipped beats, dizziness, sweating, or chest discomfort, and how long it lasts.
You can also use a smartwatch or fitness tracker to capture approximate heart rates. These are not perfect medical devices, but they give helpful trends.
Bring this log to your healthcare provider. It often speeds up getting to an answer.
Takeaway: A simple notebook or phone note can turn “my heart is weird sometimes” into useful data.
The Bottom Line: You’re Not Imagining It—and You’re Not Alone
A racing heart after eating is common and often tied to large or high-sugar meals, caffeine or alcohol, dehydration, or stress. But sometimes it is a clue to something more, like blood pressure changes, blood sugar swings, thyroid issues, or heart rhythm problems.
You do not need to panic, but you do deserve clarity. Start with small changes such as smaller, balanced meals, hydration, and less caffeine and alcohol. Track what you feel and when. Loop in a healthcare professional, especially if symptoms are new, intense, or frequent.
Your heart is doing a lot for you, all day, every day. If it is sending you signals after you eat, it is worth listening.