Feeling Unable to Take a Deep Breath: What It Might Mean and What to Do
Ever catch yourself thinking, “Why can’t I just take a deep breath?” and then immediately trying to suck in the biggest inhale of your life to prove you still can? And then it does not feel satisfying.
That can lead to mild panic, more forced breaths, and a fast trip down the “something must be seriously wrong” rabbit hole.
If that sounds familiar, you are not alone. Feeling unable to take a deep breath is a very common symptom people report to doctors, anxiety forums, and late-night search engines.
This post will walk you through what this feeling often is (and is not), common causes, what you can try at home, and when to get checked out. It is educational, not diagnostic—so if you are worried, always lean toward calling a medical professional.
What Does “Feeling Unable to Take a Deep Breath” Actually Mean?
People describe this in a few different ways:
- “I can breathe, but I cannot get a full, satisfying breath.”
- “I keep needing to yawn or sigh to feel like I got enough air.”
- “I feel like there is a block halfway down my chest.”
- “It is not exactly shortness of breath, just incomplete breathing.”
Often, oxygen levels are totally normal, and your lungs are technically working. The problem is in the sensation of breathing and the way you are using your breathing muscles.
Quick takeaway: This feeling is very real—but it does not automatically mean your lungs are failing.
Common Reasons You Might Feel Unable to Take a Deep Breath
You cannot know the cause for sure without a medical evaluation, but some patterns show up over and over.
1. Anxiety and “Air Hunger”
When your nervous system is on high alert—stress, anxiety, panic, even chronic worry—your breathing often becomes:
- faster
- shallower
- more chest-based than belly-based
This can create a sensation called air hunger or cannot get a full breath even when oxygen levels are normal.
Typical clues it might be anxiety-related:
- Symptoms get worse when you focus on your breathing or health.
- It comes in waves or episodes, often with stress or panic.
- You might also notice chest tightness, racing heart, tingling fingers or lips, or feeling on edge.
Takeaway: Your body is breathing enough, but your brain keeps pressing the “more air” button.
2. Over-Breathing and Dysfunctional Breathing Patterns
A lot of us are quietly not very good at breathing.
Modern life trains us to:
- sit slumped over laptops and phones
- breathe mostly into the upper chest
- take frequent deep sighs or yawns to “reset”
Over time, you can develop a dysfunctional breathing pattern, where you:
- overuse the neck and upper chest muscles
- underuse the diaphragm (your main breathing muscle)
- breathe faster than your body actually needs
This can make you feel like you constantly need one perfect deep breath that never quite arrives.
Takeaway: It is not always about lung capacity—sometimes it is your breathing technique.
3. Asthma or Airway Issues
Sometimes, feeling unable to take a deep breath can be related to asthma or other airway constriction problems.
Common asthma clues include:
- Wheezing (whistling sound when breathing out)
- Coughing, especially at night or with exercise
- Tight or heavy feeling in the chest
- Symptoms triggered by allergens, cold air, exercise, or infections
Other airway issues—like vocal cord dysfunction, chronic bronchitis, or exposure to irritants such as smoke and chemicals—can also make breathing feel tight or restricted.
Takeaway: If breathing trouble is triggered by exercise, allergens, or illness—or you have had wheezing—it deserves a medical workup.
4. Deconditioning and Fitness Level
If you have been more sedentary lately, your body might simply be less conditioned to handle exertion.
Signs this might play a role:
- You mainly notice the problem when walking uphill, climbing stairs, or exercising.
- You get winded faster than you used to, but basic breathing at rest is mostly okay.
- Heart and lung tests (if you have had them) come back normal.
Takeaway: Sometimes your muscles, not your lungs, are the ones complaining.
5. Post-Illness Recovery (Colds, Flu, COVID, etc.)
After a respiratory infection—anything from a basic cold to COVID—many people describe lingering:
- chest tightness
- occasional breathlessness
- an odd, unsatisfying feeling when taking a deep breath
This may be due to irritation or inflammation in the airways, muscle weakness from being sick, or increased anxiety about breathing after feeling unwell.
Takeaway: Even when you are over the infection, your breathing and energy can lag behind for weeks. Do not ignore it, but do not be surprised if recovery feels slower than the fever did.
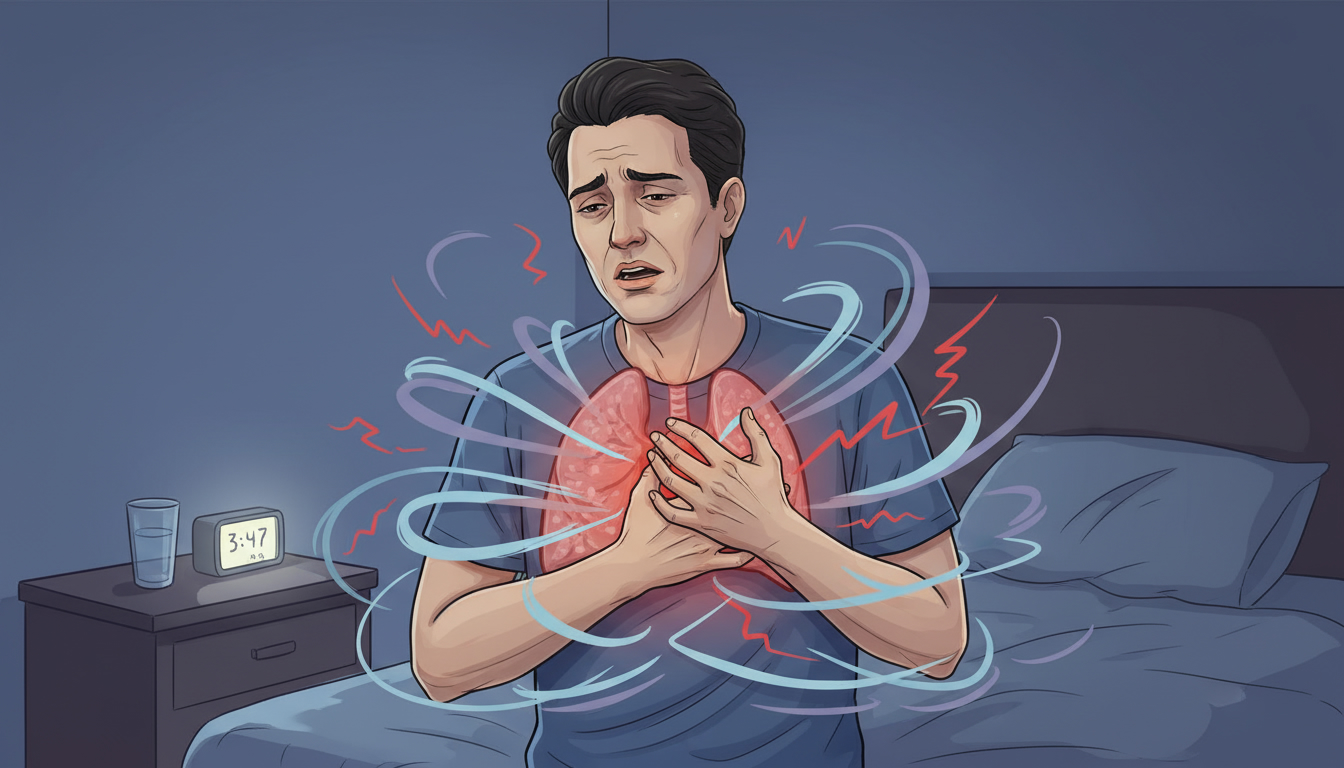
6. Heart or Lung Disease (Less Common, but Important)
While many people with the “cannot get a deep breath” sensation end up having normal testing, sometimes it can signal something more serious, like:
- heart problems (for example, heart failure, arrhythmias)
- lung disease (like pulmonary embolism, pneumonia, COPD)
- fluid around the lungs or heart
Possible red flags include:
- New or rapidly worsening shortness of breath
- Trouble breathing when lying flat; needing extra pillows
- Chest pain, pressure, or pain going to jaw, arm, or back
- Swelling in legs or sudden weight gain
- Coughing up pink, frothy, or bloody mucus
- Fever, chills, or feeling very unwell
Takeaway: These are “do not wait it out” situations. If any of these describe you, call your doctor or emergency services, depending on severity.
Is Feeling Unable to Take a Deep Breath Dangerous?
It can be, depending on what is causing it.
But many people who have this sensation have normal oxygen levels, can walk, talk, and exercise within reason, and have normal chest X-rays, ECGs, and blood tests.
In many cases the issue turns out to be anxiety, breathing pattern, or muscle tension rather than damaged lungs.
Here is a helpful question to ask yourself:
“Am I truly short of breath, or am I uncomfortable with the quality of my breath?”
If you are gasping, unable to speak full sentences, turning blue, or feeling like you are suffocating, that is an emergency.
If you are breathing, talking, and functioning but feel like your breaths are never deep enough, that is still important—but usually less immediately dangerous.
Takeaway: The brain can sound the alarm even when the numbers, like oxygen level, are totally okay.
Simple Self-Checks You Can Do Right Now (Not a Diagnosis!)
These are not to replace medical care, but they can give you a bit more information.
1. The Conversation Test
Ask yourself: Can I speak in full sentences without having to gasp for air?
- If yes, your body is likely getting enough air, even if your breathing feels strange.
- If no, or if speaking a sentence makes you very breathless, that is a sign to seek urgent help.
2. Gentle Walking Test
If it is safe for you to do so:
- Walk around your home or do a slow walk for 2–3 minutes.
- Notice: does your shortness of breath get dramatically worse? Does your chest hurt? Do you feel faint?
Severe worsening with light activity, especially if new for you, means a medical evaluation is recommended.
3. Pay Attention to Triggers
Write down:
- When you notice the feeling most (morning, night, after eating, while resting, while anxious, during exercise).
- What you are usually doing when it starts (scrolling, arguing, rushing, sitting hunched, lying down).
- Any associated symptoms (dizziness, chest pain, cough, heart pounding, and so on).
You are not doing this to self-diagnose. You are gathering data to bring to a doctor, which can speed up getting help.
Takeaway: Notice patterns, but still get real medical advice when in doubt.
How to Gently Reset Your Breathing (Practical Steps)
These strategies are generally safe for most people, but if anything makes you feel worse, stop and seek medical attention.
1. Drop Your Shoulders and Fix Your Posture
When we are stressed, we often:
- hunch forward
- tense the neck and shoulders
- lock the ribs
This literally shrinks the space your lungs have to expand.
Try this:
- Sit or stand tall, with both feet on the floor.
- Roll your shoulders up, back, and down. Let them drop.
- Imagine a string gently lifting the crown of your head.
- Place one hand on your upper chest and one on your upper belly.
Notice which hand moves more when you breathe.
Takeaway: You are giving your lungs and diaphragm physical room to do their job.
2. The 4–6 Breathing Reset
This is a calm-breathing pattern, not a competition. Avoid big dramatic inhales.
- Breathe in through your nose for a count of 4, letting your belly rise more than your chest.
- Gently breathe out through pursed lips (like blowing out a candle slowly) for a count of 6.
- Pause for 1–2 seconds before the next inhale.
- Repeat for 1–3 minutes.
Helpful tips:
- Focus on softening the breath, not deepening it.
- If 4 and 6 feel too long, do 3 in, 4 out. Comfort over perfection.
- If you feel dizzy or more panicky, stop and go back to normal, gentle breathing.
Takeaway: Longer, slower exhales can signal to your nervous system that you are safe.
3. Chest vs. Belly Experiment
Do a quick mini-experiment to retrain your brain:
- Place one hand on your chest, one on your belly.
- Take a breath where only your chest moves. Notice how shallow or tense it feels.
- Now take a breath where you try to keep your chest hand relatively still and let your belly hand rise and fall.
You are building awareness of how different breathing styles feel, so you can choose the one that supports you.
Takeaway: Belly-focused (diaphragmatic) breathing is usually more efficient and calming.
4. Limit “Checking” Breaths
If you are constantly taking big test breaths, sighing heavily, or yawning to force a deep breath, you might actually be reinforcing the feeling that your normal breathing is not enough.
Try this for a few hours:
- Allow your body to breathe however it wants, without testing or forcing big breaths.
- If you feel the urge to check, do a gentle, small inhale and an extended, slow exhale instead.
Takeaway: The more you chase that one perfect breath, the more elusive it can feel.
When Should You Seek Medical Care?
It helps to split this into urgent and non-urgent but important.
Seek Urgent or Emergency Care If You Have:
- Trouble breathing that is sudden or significantly worse than usual
- Chest pain or pressure, especially if it spreads to jaw, arm, back, or neck
- Blue or gray lips or face
- Extreme difficulty speaking full sentences
- Feeling like you might pass out, or new confusion
- Coughing up blood, or pink frothy mucus
- Very fast heart rate with shortness of breath and feeling unwell
These can be signs of serious heart or lung problems, and you should call emergency services or go to the emergency department.
Make a Non-Urgent Appointment With a Doctor If:
- You have had ongoing feelings of not getting a full breath for more than a few days or weeks.
- Exercise tolerance is dropping (you are more winded than usual doing normal things).
- You have a history of asthma, heart disease, blood clots, or lung problems.
- You recently had a COVID or respiratory infection and breathing still feels off.
- This symptom is making you anxious, interfering with sleep, or lowering your quality of life.
Your clinician may consider tests like:
- physical exam and listening to your lungs and heart
- oxygen level check (pulse oximeter)
- chest X-ray or other imaging
- ECG or heart tests
- lung function tests (spirometry)
Takeaway: You deserve reassurance and answers—not just “you are fine” with no explanation.
What If It Really Is “Just Anxiety”?
That phrase can feel dismissive—like someone is saying, “It is all in your head.” In reality, anxiety is a body-wide experience that absolutely can:
- change how your breathing muscles fire
- alter your perception of air hunger
- make harmless sensations feel terrifying
If breathing tests are normal and your provider thinks anxiety or dysfunctional breathing is the main driver, that does not mean you are making it up or that you should “just stop worrying.”
It does mean there are powerful tools that can help, including:
- breathing exercises and breath-focused physical therapy
- cognitive-behavioral therapy (CBT) or other anxiety therapies
- lifestyle changes such as movement, sleep, reducing stimulants like caffeine, and stress management
- sometimes, medication when appropriate
Takeaway: “Just anxiety” is still a real problem—and a very treatable one.
Putting It All Together
If you have been feeling unable to take a deep breath, here is the short version:
- The sensation is common and real—even when tests are normal.
- Many cases relate to anxiety, breathing patterns, posture, or recovery after illness.
- Serious causes exist, especially with red-flag symptoms—do not ignore your instinct if something feels very wrong.
- Gentle breathing resets, posture changes, and limiting test breaths may ease the feeling.
- If this is new, worsening, or worrying you, a medical check is always a good idea.
Until you get answers, try to treat yourself with the same kindness you would offer a friend who said, “My breathing feels strange and it is frightening me.”
You do not have to manage it alone—and you are allowed to ask for help.