When Is Blood Pressure Too Low?
Quick refresher: what is blood pressure, really?
Blood pressure is the force of your blood pushing against your artery walls.
It is written as two numbers:
- Systolic (top number) – pressure when your heart beats
- Diastolic (bottom number) – pressure when your heart relaxes
Example: 120/80 mmHg (read as “120 over 80”). Most people know the upper limits (like 140/90 or higher being in the high range), but the lower end gets less attention.
Key idea: Low blood pressure (hypotension) is not automatically dangerous. What matters most is how you feel and what’s causing it.
Takeaway: The numbers are important. The symptoms are more important.
So… what counts as low blood pressure?
In many guidelines, hypotension is often defined as below 90/60 mmHg. But that number alone does not equal an emergency.
Some people, especially young, healthy adults or endurance athletes, naturally run low, like 95/60 or even a bit lower, and feel completely fine.
You might be in the “low but normal for you” camp if:
- You have always had lower readings
- You have zero symptoms (no dizziness, no fainting, no unusual fatigue)
- Your doctor is not worried and your labs and exam are normal
In that case, low-ish numbers can actually be a good thing for long-term heart health.
Takeaway: A low reading on paper is only a problem if your body is acting like it is a problem.
When is blood pressure too low?
Blood pressure is “too low” when it does not get enough blood and oxygen to your organs. That is when you start getting symptoms.
Common red-flag symptoms include:
- Dizziness or feeling lightheaded
- Blurry or tunnel vision
- Fainting or almost fainting
- Fatigue or weakness that does not make sense
- Confusion, trouble concentrating
- Nausea
- Cold, clammy, or pale skin
- Fast, shallow breathing
- Rapid, weak pulse
Now add the numbers:
- A blood pressure like 80/50 with lightheadedness is concerning.
- A sudden drop from 130/80 to 90/60 with symptoms is also concerning, even though 90/60 is on the “borderline normal” list.
Takeaway: The change in blood pressure and the symptoms matter more than one single reading.
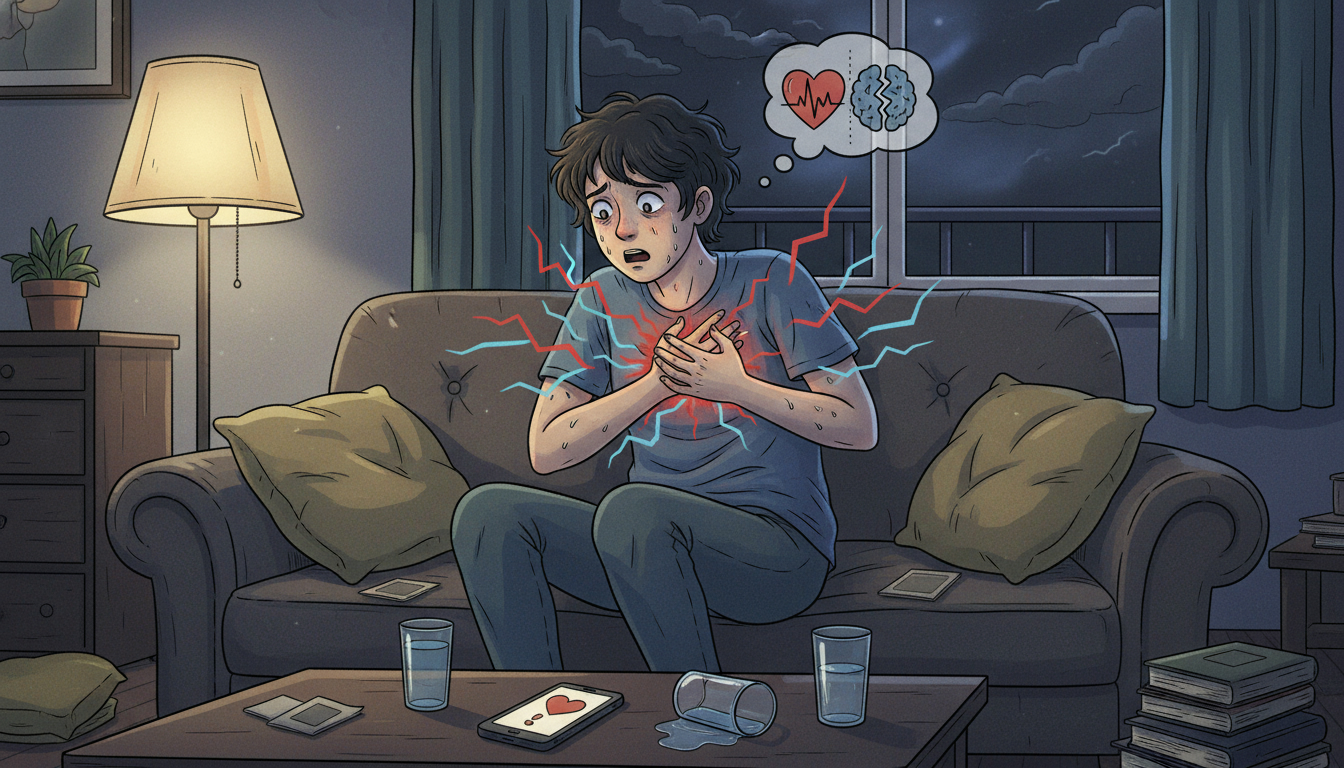
Serious warning signs: when to call emergency services
If low blood pressure shows up with any of these, it can be an emergency:
- Chest pain or pressure
- Shortness of breath
- Confusion, trouble speaking, acting “off” mentally
- Fainting and not waking up quickly
- Blue or gray lips or fingers
- Very fast heart rate, especially with weakness
- Signs of severe allergic reaction (hives, swelling of lips or tongue, trouble breathing)
- Vomiting, diarrhea, or bleeding plus feeling like you might pass out
This can happen with things like severe dehydration, internal bleeding, sepsis (serious infection), heart problems, or a severe allergic reaction.
If you are experiencing these right now: stop reading and call emergency services. This article is not a substitute for urgent medical care.
Takeaway: Low blood pressure plus serious symptoms is not a “wait and see” situation.
What causes low blood pressure?
Low blood pressure can be grouped into two big categories: occasional dips and chronic low blood pressure.
Occasional or sudden low blood pressure
These are scenarios where your blood pressure may crash temporarily:
-
Standing up too fast (orthostatic hypotension)
Standing up and suddenly feeling like your brain forgot to come with you is often orthostatic (postural) hypotension, when your blood pressure drops as you go from lying or sitting to standing.
-
Dehydration
Not enough fluid in your blood means lower volume and lower pressure. Add heat, sweating, vomiting, or diarrhea, and it can drop fast.
-
Blood loss
From injury, surgery, internal bleeding, or heavy menstrual bleeding, losing blood means losing volume and pressure.
-
Medications
Common culprits include:
- Blood pressure medications
- Diuretics (“water pills”)
- Some antidepressants
- Medications for Parkinson’s disease
- Some heart medications
-
Severe infection (sepsis)
In sepsis, blood vessels widen and leak, and pressure can plummet.
-
Severe allergic reactions (anaphylaxis)
Allergic reactions can cause blood vessels to open wide and blood pressure to drop.
Chronically low blood pressure
Some people run low all the time. Other times, it is linked to:
- Hormonal issues such as adrenal or thyroid problems
- Heart conditions such as very slow heart rate, heart failure, or heart valve problems
- Nervous system disorders where conditions affect the nerves that control blood vessel tone and heart rate
Takeaway: A one-off low reading after you skipped breakfast is very different from weeks of dizziness and fatigue.
Is my blood pressure too low if I feel fine?
Probably not.
If your blood pressure is, for example, 95/60 or even 88/58, but you feel totally normal, can exercise without unusual symptoms, are thinking clearly, and your doctor has checked you out and is not concerned, then that might just be your body’s natural setting.
Lower pressure without symptoms is often associated with lower risk of heart disease and stroke over time.
Takeaway: If you have low numbers but high quality of life, your body might just like running in energy-saver mode.
But what if I do not feel fine?
If your blood pressure is low and you are having symptoms, that is worth a conversation with a health professional.
They may:
- Ask about your medications, supplements, and alcohol intake
- Check for dehydration or blood loss
- Ask about recent illnesses, infections, or fevers
- Review your heart history and family history
- Possibly run tests like blood work, ECG, or other studies depending on your situation
Takeaway: Symptomatic low blood pressure deserves real-life medical attention, not just an online search.
What you can do right now if your blood pressure runs low
This is general information, not personal medical advice, but these are common strategies doctors often recommend for people with non-dangerous, chronic low blood pressure.
1. Hydrate like it is your job
Low blood volume means low blood pressure.
- Sip water through the day, not just in big, occasional gulps.
- On hot days or when you are more active, increase fluids.
- If your doctor says it is okay, drinks with electrolytes can help too.
2. Do not skip meals
Blood sugar dips can make low blood pressure feel worse.
- Eat regular meals and snacks with protein and complex carbohydrates.
- Avoid huge heavy meals that make you sleepy and sluggish; they can pull blood into your digestive system and leave you lightheaded.
3. Stand up smart
If you tend to get dizzy when standing:
- Move from lying to sitting to standing, instead of jumping straight up.
- Flex your calf muscles before you stand by wiggling or marching in place a bit.
- Take a second after standing before you walk.
4. Dress and sleep strategically
Depending on your situation and your doctor’s advice:
- Compression stockings or abdominal binders can help keep blood from pooling in your legs.
- Some people feel better sleeping with the head of the bed slightly elevated.
5. Ask about salt (do not do this on your own)
In some people with low blood pressure, doctors may recommend slightly higher salt intake, but this is not for everyone.
- If you have heart disease, kidney disease, or are at risk for high blood pressure, more salt can be dangerous.
- Never make big changes to salt intake without asking a professional who knows your health history.
6. Review your medications with your doctor
If your blood pressure dropped after starting or changing a medication, that is important to mention.
- Do not stop prescription medications on your own.
- Do ask whether a medication could be lowering your blood pressure too much.
Takeaway: Small changes to fluids, food, posture, and habits can make a big difference, but they should be tailored to you.
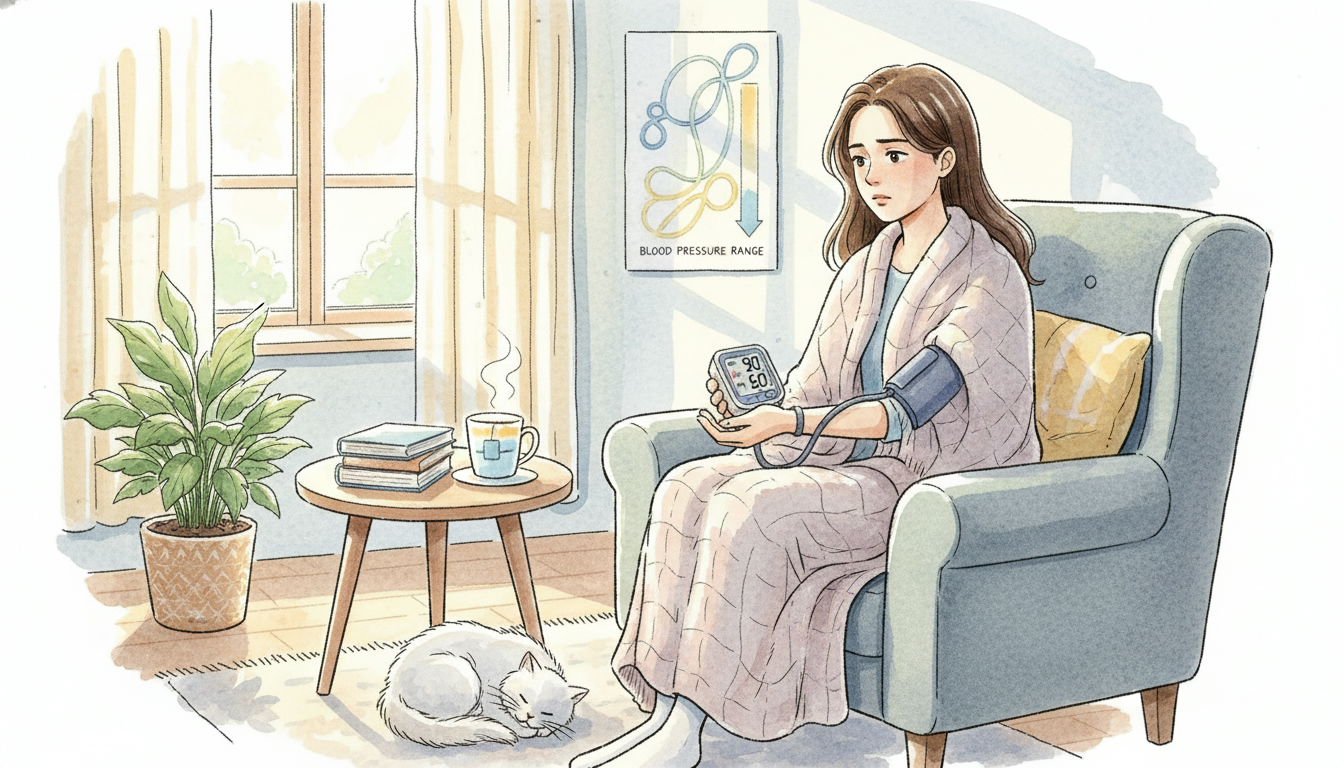
How (and when) to check your blood pressure at home
Home monitors can be very helpful if you use them correctly.
How to get more accurate readings
- Sit quietly for 5 minutes before measuring.
- Keep your feet flat on the floor, back supported, and arm at heart level.
- Do not smoke, drink caffeine, or exercise within 30 minutes before.
- Use the right cuff size for your arm.
Take readings at different times of day and keep a log with:
- Date and time
- Reading (for example, 98/62)
- How you felt (fine, dizzy, tired, and so on)
Bring that log to your appointments. It gives your doctor actual data instead of “I think it is low sometimes.”
Takeaway: One random reading does not tell the whole story; patterns do.
FAQ: common questions about low blood pressure
Can low blood pressure make me tired?
Yes. If your organs, including your brain and muscles, are not getting enough blood and oxygen, you may feel wiped out, weak, or foggy.
Can low blood pressure cause anxiety or feel like anxiety?
It can. Dizziness, racing heart, and feeling like you might faint can feel like a panic attack. Sometimes low blood pressure and anxiety even show up together. That is why it is important to get checked instead of guessing.
Is low blood pressure dangerous in pregnancy?
Blood pressure often drops in early to mid-pregnancy because blood vessels relax and your circulatory system expands. Many pregnant people feel a bit lightheaded at times.
However, any dizziness, fainting, chest pain, shortness of breath, severe headaches, or visual changes in pregnancy should be discussed with an obstetrician or midwife right away.
Can I exercise if my blood pressure is low?
Often, yes. Exercise can actually help your body regulate blood pressure better over time. But if you are fainting, getting chest pain, or feeling extremely short of breath, that needs medical evaluation first.
Takeaway: If a “simple” symptom like dizziness keeps showing up, it deserves a real conversation with a professional.
The bottom line: when is blood pressure too low?
Think of it this way:
- Low number + no symptoms + normal checkup → often okay, maybe even ideal
- Low number + mild symptoms (dizzy, tired, fuzzy) → talk to your doctor soon
- Low number + severe symptoms (chest pain, confusion, trouble breathing, severe weakness, fainting) → seek emergency care
Your body is allowed to have its own “normal,” but it is not supposed to make you miserable or unsafe getting there.
If you are worried about your readings or how you feel, write down:
- Your recent blood pressure numbers
- When symptoms happen
- Any new medications, illnesses, or changes in your life
Then bring that list to your next appointment and say, “I am worried my blood pressure might be too low — can we walk through this together?” That question alone is a strong start.