
Panic Attack vs Heart Attack: How to Tell the Difference
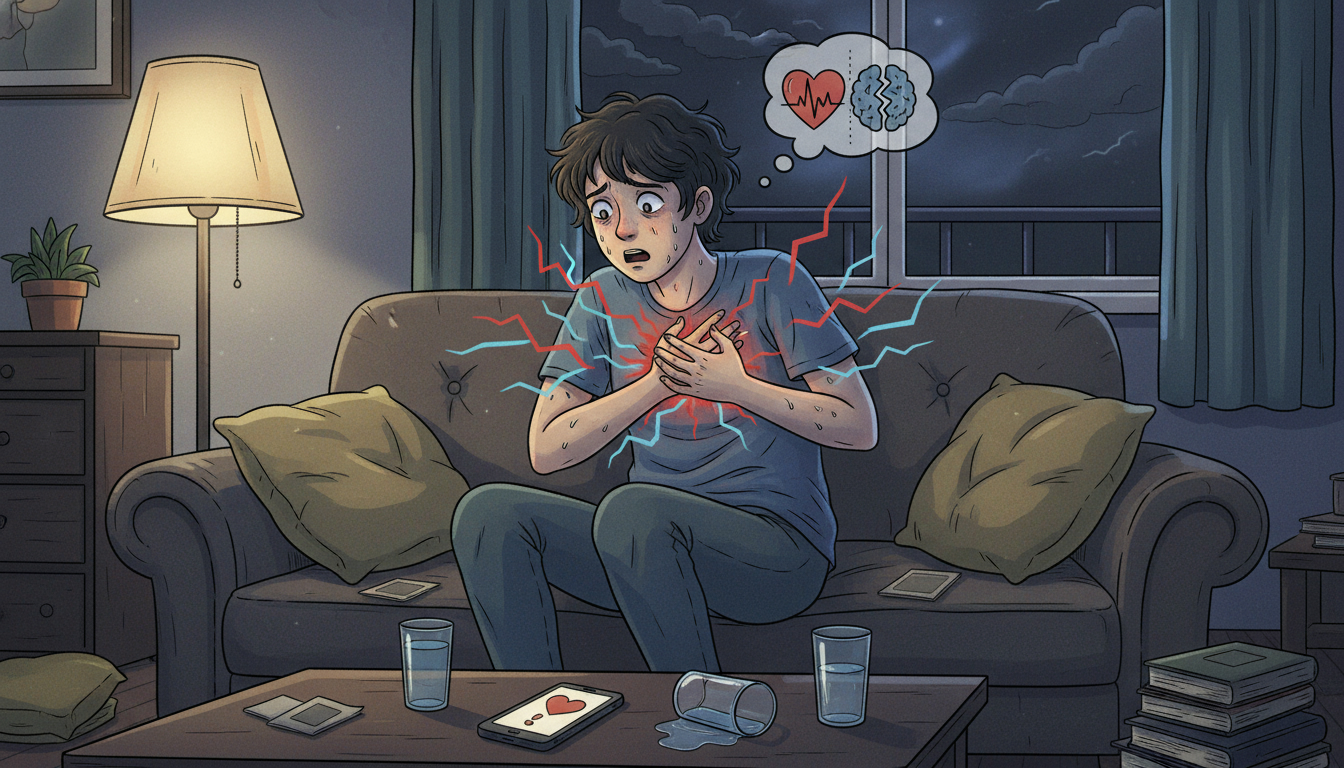
You are sitting on the couch, scrolling your phone, when it hits: your chest feels tight, your heart is racing, you are sweating, dizzy, and suddenly very aware of your own mortality.
One thought crashes through your brain: “Am I having a heart attack or just a panic attack?”
If you have ever had that moment, you know it is terrifying. And to make it worse, panic attacks and heart attacks can feel shockingly similar.
This guide will walk you through:
- The key differences between a panic attack and a heart attack
- Common symptoms of each
- Red-flag signs that mean you should call 911 right now
- What to do in the moment when you cannot tell which it is
This is not a DIY diagnostic tool. It is a clarity-and-calm guide so you are not completely in the dark when your body is reacting strongly.
Important: If you think you might be having a heart attack, treat it like a heart attack and call 911. It is always better to be checked and told “you are okay” than the other way around.
Panic attack vs heart attack: Why they are so easy to confuse
Let us start with the overlap.
Both panic attacks and heart attacks can cause:
- Chest pain or discomfort
- Racing or pounding heart
- Sweating
- Shortness of breath
- Nausea or stomach upset
- Feeling like something is very wrong (impending doom)
The difference is mainly in what is happening in your body and the pattern of symptoms over time:
- A heart attack happens when blood flow to part of your heart is blocked. This can damage heart muscle and is a medical emergency.
- A panic attack is a surge of intense fear or discomfort, often triggered by stress or sometimes appearing “out of nowhere.” Your body goes into fight-or-flight mode: adrenaline, fast breathing, and a racing heart.
Key takeaway: The feelings can overlap, but a heart attack is a plumbing problem in your heart; a panic attack is more like your alarm system going into overdrive.
What is a panic attack?
A panic attack is a sudden episode of intense fear or discomfort that peaks within minutes. Panic attacks often include physical symptoms that can feel life-threatening, even when they are not.
Common panic attack symptoms include:
- Racing or pounding heart
- Chest pain or tightness
- Shortness of breath or feeling like you cannot get enough air
- Sweating or chills
- Trembling or shaking
- Nausea or stomach distress
- Dizziness or feeling faint
- Numbness or tingling (especially in hands, feet, or face)
- Feeling detached from reality (“this does not feel real”)
- Fear of losing control or “going crazy”
- Fear of dying
How panic attacks usually behave
While everyone is different, panic attacks often:
- Come on suddenly and peak within 10 minutes, then gradually ease over 20–30 minutes (sometimes longer)
- May be linked to stress, phobias, social situations, or sometimes happen “out of the blue”
- Can leave you exhausted but usually do not cause physical damage to the heart in otherwise healthy people
You might notice a pattern over time: similar triggers, similar sensations, and similar “I survived that” endings.
Mini-takeaway: Panic attacks feel dangerous, but they are usually not physically dangerous. However, you should never assume chest pain is “just anxiety” without a medical evaluation.
What is a heart attack?
A heart attack (myocardial infarction) happens when one of the arteries that supply blood to your heart gets blocked. This can damage or destroy part of the heart muscle and is a medical emergency.
Heart attacks are a leading cause of death, but getting rapid treatment (ideally within the first 1–2 hours of symptom onset) dramatically improves outcomes.
Common heart attack symptoms include:
- Chest discomfort: pressure, squeezing, fullness, or pain in the center or left side of the chest that lasts more than a few minutes or goes away and comes back
- Pain or discomfort radiating to one or both arms, back, neck, jaw, or upper stomach
- Shortness of breath (with or without chest discomfort)
- Cold sweat
- Nausea, vomiting, or indigestion-like discomfort
- Lightheadedness or sudden dizziness
Heart attack patterns to know
Heart attack symptoms can:
- Come on suddenly and intensely (the classic movie-style clutching the chest)
- Or start slowly with mild pain or discomfort that builds over minutes to hours
Not everyone has “crushing” chest pain. Some people, especially women, older adults, and people with diabetes, may have more subtle or atypical symptoms like:
- Unusual fatigue
- Shortness of breath
- Pressure or discomfort in the back, jaw, or shoulders
- A feeling of “I just do not feel right” that will not go away
Mini-takeaway: Heart attacks are not always dramatic, but they are always an emergency. If in doubt, get checked.
Panic attack or heart attack? Key differences you might notice
You cannot safely self-diagnose a heart attack at home. But understanding patterns can help you know when to be extra cautious.
Think of these as clues, not rules.
1. Type and location of chest pain
Panic attack:
- Often sharp, stabbing, or very tight
- May stay in one small area of the chest
- Can worsen when you focus on it or take very deep breaths
Heart attack:
- More often described as pressure, squeezing, fullness, or heavy pain
- Usually in the center or left side of the chest
- May radiate to the arm, neck, jaw, back, or upper stomach
2. Trigger and timing
Panic attack:
- Frequently linked to stress, fear, crowds, confined spaces, or health worries
- Often starts suddenly and peaks quickly (within about 10 minutes)
Heart attack:
- Can occur during physical exertion, emotional stress, or even at rest or during sleep
- Symptoms may build slowly over minutes or hours and keep going or cycling
3. Breathing and sensations
Panic attack:
- You may feel like you cannot get enough air and start breathing fast
- Tingling in hands, feet, or around the mouth is common (from over-breathing)
- You may feel detached, unreal, or like you are watching yourself
Heart attack:
- Shortness of breath might appear with or without chest pain
- Less likely to cause tingling in hands or face from breathing changes
- More likely to be paired with cold sweats, nausea, or radiating pain
4. Duration
Panic attack:
- Intensity usually peaks within 10 minutes, then gradually lessens
- You may feel “off” for a while afterward but the worst part passes
Heart attack:
- Discomfort usually lasts more than a few minutes, may go away and return
- Often does not fully resolve without medical treatment
5. Risk factors
These do not decide what you are having, but they matter.
Heart attack risk goes up with:
- Age (especially 45+ for men, 55+ for women)
- Smoking
- High blood pressure, high cholesterol, or diabetes
- Obesity or sedentary lifestyle
- Family history of early heart disease
Panic attacks are more common with:
- History of anxiety or panic disorder
- Recent major stress or trauma
- Thyroid problems or certain medications (as triggers)
- Family history of anxiety disorders
Mini-takeaway: Patterns can hint at what is going on, but never use this list to talk yourself out of calling 911 if something feels seriously wrong.
Real-life style scenarios
Sometimes it is easier to recognize patterns in stories. These are examples, not rules.
Scenario 1: The sudden wave at the grocery store
You are standing in line. Out of nowhere, your heart starts pounding. Your chest feels tight. Your hands tingle, you feel dizzy, like you might pass out. You are suddenly terrified you will collapse in front of strangers.
Within 10–15 minutes, the worst of it passes. You feel shaky, drained, and embarrassed.
This pattern, sudden onset, intense fear, tingling, and relatively quick peak, fits more with a panic attack. But if this is your first time with chest pain, it is still reasonable to get evaluated.
Scenario 2: The slow burn while watching TV
It is evening and you are relaxed. You notice a pressure in the center of your chest. It is not stabbing, but it feels like something is sitting on your chest. After 20 minutes, it is still there.
Then you notice it is starting to spread into your left arm and jaw. You are a 58-year-old with high blood pressure and high cholesterol.
This pattern, pressure-type pain, lasting longer than a few minutes, radiating to arm and jaw, plus risk factors, is very concerning for a heart attack.
That is a call 911 immediately situation.
Scenario 3: The workout confusion
You are on the treadmill. You feel chest discomfort and shortness of breath. When you stop, the pain eases a bit but does not fully go away. You are 45, you smoke, and heart disease runs in your family.
Even if you have a history of anxiety, this must be treated as potential heart trouble until proven otherwise.
Mini-takeaway: If there is any reasonable chance it is your heart, get emergency help. Anxiety can be treated; a missed heart attack can be fatal.
When to call 911 immediately
Use this as your “do not overthink it, just act” list.
Call 911 (or your local emergency number) right away if:
- You have chest pain, pressure, squeezing, or discomfort that:
- Lasts more than a few minutes, or
- Goes away and comes back
- The pain spreads to your arm, back, neck, jaw, or upper stomach
- You have chest discomfort plus:
- Shortness of breath
- Cold sweat
- Nausea or vomiting
- Lightheadedness or fainting
- You feel an unexplained sense of doom or “about to die” with chest symptoms
- You have heart disease, are older, or have risk factors, and the symptoms are new or more intense than usual
If you are with someone and they collapse, complain of severe chest pain, or seem to be having a heart attack, call 911 first, then follow the operator’s guidance.
Mini-takeaway: In a real emergency, seconds matter more than pride. No one in the ER will be upset that you came in to be checked.
What to do right now if you are not sure
If you are having symptoms as you read this and feel unsure, here is a calm step-by-step:
- Check your gut and the red flags.
- Severe, crushing, pressure-like chest pain? Radiating to arm or jaw? Short of breath, nauseous, sweaty? Call 911.
- If symptoms are milder but scary and new, especially with risk factors (age, blood pressure, cholesterol, smoking, family history), it is still wise to seek urgent care or ER evaluation.
- If you have been evaluated before for similar symptoms and told it was panic or anxiety, but this episode feels different, stronger, or you are not sure, err on the side of getting checked again.
- While you wait for help or if a clinician has already ruled out a heart issue and says it is likely panic, try grounding:
- Slow breathing: inhale for 4 seconds, exhale for 6 seconds. Repeat.
- The 5–4–3–2–1 technique: name 5 things you see, 4 you can touch, 3 you hear, 2 you smell, 1 you can taste.
- Remind yourself: “I have felt like this before and survived. This wave will pass.”
Mini-takeaway: When you cannot tell if it is panic or heart, you treat it as heart until a medical professional says otherwise.
Long-term: Dealing with recurring panic attacks
If you have been told by a healthcare professional that your heart is healthy and your episodes are panic attacks, the next step is management and prevention, not just enduring each one.
Evidence-based options include:
- Cognitive behavioral therapy (CBT): Helps you understand and rewire the thoughts and body-sensations spiral that leads to panic.
- Exposure-based therapy: Gradually and safely exposes you to sensations or situations that trigger panic, so they become less terrifying.
- Medication: Some people benefit from SSRIs or other medications; this is a conversation with a healthcare provider or psychiatrist.
- Lifestyle foundations:
- Regular movement (even walking)
- Limiting caffeine and alcohol
- Prioritizing sleep
- Stress-management practices (meditation, breathing exercises, journaling)
If panic attacks are affecting your work, relationships, or ability to leave the house, it is absolutely worth getting professional help. Panic disorder is very treatable.
Mini-takeaway: If your heart is okay but your anxiety is not, that is still real, and you deserve support.
When you have already had a heart attack or heart scare
If you have previously had a heart attack, stent, or other heart condition, new chest symptoms can trigger panic on top of real physical sensations. That is incredibly stressful.
Important steps in that situation:
- Work closely with a cardiologist and primary care clinician.
- Ask them to explain your specific warning signs and when to go straight to the ER.
- Consider cardiac rehab programs; they often address both physical and emotional recovery.
- Ask about mental health support. Anxiety and depression are common after cardiac events and treating them can improve quality of life.
Mini-takeaway: Heart history plus anxiety is a double load. You do not have to carry it without a team.
The bottom line: You do not have to guess alone
Here is a simple summary:
- Panic attacks and heart attacks share symptoms, especially chest pain, racing heart, and shortness of breath.
- Panic attacks usually come on quickly, peak within minutes, and often include intense fear, tingling, and a feeling of unreality.
- Heart attacks more often involve pressure-type chest pain, may radiate to the arm, jaw, or back, and do not fully let up without treatment.
- Risk factors (age, blood pressure, cholesterol, smoking, family history) increase the odds a symptom is heart-related.
- If you are not sure, treat it as a heart emergency and call 911.
You are not being “dramatic” for taking your health seriously.
If you have had repeated scares, whether they turned out to be panic, heart issues, or both, this is your nudge to:
- Schedule a check-in with a healthcare professional
- Talk openly about both physical and mental health
- Create a clear plan for what to do if it happens again
That way, the next time your chest tightens and your thoughts spiral, you will have more than fear, you will have a plan.
Disclaimer: This article is for general information and education only. It is not a substitute for personal medical advice, diagnosis, or treatment. If you have concerning symptoms, especially chest pain or trouble breathing, seek emergency care immediately.
Leave a Reply